MENUMENU
Arizona Medicaid is a government-run healthcare program that provides health insurance coverage to low-income individuals who cannot afford private health insurance. Medicaid covers a wide range of medical treatments, procedures, and specialists.
Another name for the Arizona Medicaid program is Arizona Health Care Cost Containment System (AHCCCS). Approximately one in every three Arizonans has coverage under Arizona Medicaid, bringing the total number of covered Arizonans to over 2.5 million. The healthcare services are delivered by more than 115,000 qualified medical professionals in the state.
Arizona Medicaid allows eligible individuals to choose programs that fit and are available in their ZIP code and location. Program members choose a doctor that accepts Medicaid to provide medical services, treatments, and medication. Your primary care doctor also provides referrals to specialists. Two of the most common questions posed to AHCCCS are:
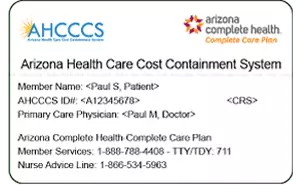
An AHCCCS card contains your unique Arizona Medicaid ID number. Your ID number confirms you are a member of the AHCCCS healthcare program, requiring you to present the card to healthcare providers when you get healthcare services.
It is illegal to share your card with other people, an act that could constitute Medicaid fraud. Your Medicaid card has all relevant information about your account, including your Medicaid ID number, date of birth, sex, and card number.
You can apply for Arizona Medicaid online at their official website here. You can also print an application, complete it, and send it via mail or fax it to a regional Medicaid office. You can also work with a Community Assistor if you need assistance applying for the program. You can find an assistor here to help you apply.
After applying, the Medicaid office might contact you for extra documents to prove eligibility. Most people will hear a response about approval within 45 days. If you are pregnant, you will hear back in 20 days, and if you are in the hospital, you will hear back within seven days. If you are denied approval and you believe the ruling to be in error, you can appeal the decision. It normally takes 30 days to process an application rejection appeal.
Arizona Medicaid eligibility is based on income limits. Income limits for eligibility differ between adults and children from low-income homes. Please consult the table below, which shows the income limits and special eligibility requirements for children and adults.
| Applicants | Income Limits(per Household Member Number) | Special Requirements |
|---|---|---|
| Children under 1 | 1. $1,787 2. $2,416 3. $3,046 4. $3,675 ($630 per additional person) | None |
| Children 1-5 | 1. $1,714 2. $2,318 3. $2,922 4. $3,525 ($604 per additional person) | None |
| Children 6-18 | 1. $1,616 2. $2,166 3. $2,756 4. $3,325 ($570 per additional person) | None |
| Children under 19 | 1. $2,430 2. $3,287 3. $4,144 4. $5,000 ($857 per additional person) |
|
| Adults | 1. $1,616 2. $2,186 3. $2,756 4. $3,325 ($455 per additional person) |
|
| Pregnant women | 1. $1,896 2. $2,564 3. $3,232 4. $3,900 ($669 per additional person) | None |
| Caretaker relatives | 1. $1,288 2. $1,742 3. $2,196 4. $2,650 ($455 per additional person) | None |
| Long-term care | 1. $1,288 2. $1,742 3. $2,196 4. $2,650 ($455 per additional person) |
|
To view the AHCCCS eligibility requirements chart online as of February 1, 2023, click here.
Income includes regular employment income, alimony payments, pensions, social security, stock dividends, and IRA withdrawals. Countable assets include cash, vehicles, homes, stocks, investments, and savings accounts. For patients receiving long-term care, Arizona can perform estate recovery to recover any spent funds if the recipient passes away.
Lying about your income on Medicaid applications is considered fraud. If you are accepted into a plan and the state discovers you misrepresented key eligibility information, you can lose your health insurance coverage and possibly be required to pay back all expenditures provided by the state.
It’s important to note that Arizona Medicaid may not provide enough coverage in an instance where someone becomes temporarily or permanently disabled. Investing in quality disability insurance is an excellent way to assist with some of the costs incurred with not being able to work, and to help with the cost of medical needs.
You should receive an Arizona Medicaid card in the mail after you are approved for the program and have applied through the correct channels. Depending on the type of benefits you apply for, the wait times to receive a card may vary. The chart below provides wait time guidelines.
| Application Type | Approximate Waiting Period |
|---|---|
| MSP | 45 days from date of application |
| BCCTP | 7 days from date of application |
| SSI-MAO (disability) | 90 days from date of application |
| Pregnancy & Requiring Medical | 20 days from date of application |
| Hospitalized | 7 days from date of application (Time frame only applicable if no other documentation is required) 45 days from date of application (if additional documentation is required) |
| Other Programs (all) | 45 days from date of application |
If you need medical care in the meantime, you can present your Medicaid acceptance letter with your ID number to your healthcare provider. You can also find your Medicaid ID number on your AHCCCS account dashboard, or you can give your healthcare provider your social security number to look up your Medicaid account. You cannot access Medicaid services if you do not have a Medicaid ID number.
You must renew your Arizona Medicaid status every year. The state office will review your income from your previous application and make an approval judgment. If the state office cannot determine eligibility from your previous application, they will send a request for documents proving your eligibility. You must complete this form by the specified date, or else you may lose AHCCCS coverage. It is highly advisable to create an AHCCCS account in order to update your contact information to receive renewal notifications on time. You can also sign up for text or email alerts. If you are not eligible for your current program, the state office will screen your eligibility for other medical assistance programs.
If you have lost your AHCCCS member card, you can get a new one by contacting your health plan provider. Arizona does not charge to replace Medicaid cards. Depending on the type of AHCCCS coverage you have, the phone number to report a lost or damaged card may vary. For a complete list of AHCCCS providers and their contact numbers, click here.
In addition to providing comprehensive healthcare coverage, Arizona Medicaid, also known as AHCCCS, offers a broad array of medical services to eligible individuals. The coverage includes both emergency and routine health services, ensuring that beneficiaries have access to essential treatments. From preventive care and doctor visits to hospital stays and prescription medications, Arizona Medicaid covers a wide range of healthcare needs. However, it's important to note that there may be certain treatments or services that are not covered by the program. It is essential to familiarize yourself with the specific coverage guidelines and limitations to fully understand what treatments are included and what may require alternative sources of funding. By exploring the details of Arizona Medicaid coverage, you can make informed decisions about your healthcare options and ensure that you receive the necessary care.
Arizona Medicaid provides emergency and preventative dental care for children under the age of 20 years old. Arizona recently expanded AHCCCS dental coverage to include emergency dental services for adults 21 years of age or older. Annual limits for emergency dental procedures are $1,000. The list below details the coverage types within the AHCCCS plan.
For children under the age of 21, AHCCCS covers a variety of dental services including:
For those over the age of 21, AHCCCS covers:
For those who have more serious dental issues and anticipate requiring more visits to the dentists, investing in private dental plans in Arizona is advisable.
Arizona Medicaid covers most generic prescription drugs that are prescribed by a physician. Most AHCCCS members pay a $2.30 co-payment per prescription. You do not have to pay a co-payment if:
The drugs on Arizona’s preferred drug list (PDL) do not require prior authorization unless they are for a recipient under six years old. Arizona Medicaid requires generic substitutions where available. If brand drugs are medically necessary, you can get prior authorization to cover those prescriptions.
More specifically, Arizona Medicaid recipients can receive up to a month’s worth of prescription medication per co-payment. You must use at least 90% of controlled substances and 85% of non-controlled substances before you can refill a prescription. If you require medically necessary prescriptions and a physician is unavailable, AHCCCS will allow a one-time five-day supply dispensal.
Rehabilitation services, nursing facilities, and home care often require long-term aid. AHCCCS alleviates these health costs and covers many aspects of extended health care. From senior services like living in a nursing home or having an in-home nurse may fall under the umbrella of Arizona Medicaid. AHCCCS requires individuals to meet certain criteria to qualify for extended health care, such as having a proven developmental or intellectual disability. Arizona Medicaid may also approve service authorizations for elderly patients requiring a stay in a long-term health care facility. Additional services that are covered for eligible individuals under the AHCCCS are:
AHCCCS has two programs that provide extended medical benefits for Arizona Medicaid recipients. These programs provide additional coverage to individuals and families who need additional assistance outside of regular AHCCCS coverage.
TMA coverage is for families previously receiving AHCCCS coverage and who have lost eligibility due to increased income. During the transition into self-supporting work, TMA is available for 12 months, provided the state reviews the household’s status after the first six months. To qualify for the remaining six months, all of the following must be true:
In AHCCCS (Arizona Medicaid), the Medicaid Guaranteed Enrollment Period is a specific time frame during which individuals who qualify for Medicaid can enroll in a health plan. The Guaranteed Enrollment Period ensures that eligible individuals have the opportunity to select a health plan that meets their needs. During this period, individuals can choose a health plan without being subject to any restrictions or limitations based on their health status or medical history. The exact duration of the Medicaid Guaranteed Enrollment Period may vary, so it is important to check with AHCCCS or the Medicaid agency in Arizona for the most up-to-date information.
AHCCCS members can still receive coverage out of state if they require medically necessary services. Out-of-state AHCCCS members can receive coverage if any of the below are true:
Please note that these provisions only apply to out-of-state coverage and do not apply to services received outside of the country.
On the other hand if you are traveling out-of-state for leisure and you require medical attention, chances are your Arizona Medicaid won’t cover your expenses. In some cases, if heaven forbid a life-threatening emergency occurs, AHCCCS may kick in, but this is on a case-by-case instance. If you are traveling outside of Arizona for leisure, invest in proper travelers insurance.
Arizona Medicaid has the School-Based Claiming Program that reimburses school-based providers for services they render to students who are eligible under Title XIX protections.
Seniors over the age of 65 are also eligible for Arizona Medicaid as well as Medicare. AHCCCS members who also receive Medicare are dual eligible members. Dual eligible members can have a single plan that coordinates all their care into a single network of providers. If your plans are not aligned, you can change your plan to a Dual Eligible Special Needs Plan (D-SNP) that provides additional coverage for things like dental and vision.
AHCCCS offers Medicaid for subgroups the same way it offers medicaid to every other eligible person in the state, though the path to receive coverage may be slightly different. The discussion below outlines coverage for American Indians and Military personnel.
American Indians who fall under the umbrella of eligibility for AHCCCS may enroll in any of the Complete Care plans which are associated with their specific circumstance. For those who are physically disabled and or elderly, there may be an opportunity to qualify for the Tribal Arizona Long Term Care System. A complete overview of the (TALCS) can be found here.
AHCCCS (Arizona Medicaid) does not provide healthcare coverage for individuals in the military. Healthcare for military personnel, veterans, and their families is typically provided through the TRICARE program. TRICARE is the healthcare program for uniformed service members, retirees, and their dependents, including eligible family members. It is separate from AHCCCS and is administered by the Department of Defense. If you are in the military or a military family member seeking healthcare coverage, it is advisable to explore the options available through TRICARE to ensure you receive the appropriate benefits and services.
AHCCCS exists to provide necessary medical care to children and adults who meet the criteria to gain approval for receiving Arizona Medicaid coverage. To ensure that the insurance only applies to approved procedures, Medicaid won’t cover some medical procedures and equipment, including:
If you are not sure whether Medicaid will cover a specific procedure, contact your health plan provider for information.
Healthcare in the US is complex, and even if you are on Arizona Medicaid, it can be difficult to know what, exactly, the plan will cover. In this section, we will go over common medical treatments and procedures and discuss whether they are covered under AHCCCS.
| Dental | |
|---|---|
| X-rays and exams | Arizona Medicaid covers emergency and preventative dental services for children under the age of 20, including X-rays and oral exams. AHCCCS will also cover emergency dental services for recipients over the age of 21. AHCCCS does not cover routine dental care for those over 21 years old. |
| Wisdom teeth | Arizona Medicaid will cover wisdom teeth extraction for adults over 21 if it is a medically necessary surgery. AHCCCS will not cover wisdom teeth extraction for non-emergency reasons. |
| Vision | |
|---|---|
| Eye Exams | Arizona Medicaid covers regular eye exams and screenings for recipients under 21 years of age. It does not provide regular vision care for recipients over 21 years of age. |
| Glasses | Arizona Medicaid will cover prescription glasses and glasses replacement for children under the age of 21. It will not cover prescription glasses for recipients over 21 unless their vision problems are a result of cataract surgery. |
| Laser Eye Surgery | Arizona Medicaid will not cover LASIK eye surgery because it is an elective procedure. |
| Surgery | |
|---|---|
| Rhinoplasty | Arizona Medicaid will not cover an elective rhinoplasty, but it will cover medically necessary rhinoplasty procedures due to a broken nose, nasal deformity, or other medical conditions. |
| Breast Reduction | AHCCCS does not typically cover breast reduction as it is usually considered a cosmetic procedure. Arizona Medicaid will cover a breast reduction if a doctor says it’s medically necessary. AHCCCS will also cover breast reconstruction surgery after receiving a medically necessary mastectomy. |
| Hospital | |
|---|---|
| Hospital stays | AHCCCS will pay for any inpatient or outpatient hospital care. There is no limit to the number of inpatient or outpatient days of treatment. |
| Ambulance transportation | AHCCCS will cover non-emergency ground ambulance transportation that is medically necessary. |
| Giving birth | AHCCCS covers labor and delivery services from a Licensed Midwife. C-sections are also covered if they are medically necessary. |
| Sexual Health | |
|---|---|
| Gynecologist visits | Gynecology. AHCCCS covers regular gynecological exams and services. |
| Erectile Dysfunction | Arizona Medicaid will not cover drugs for sexual or erectile dysfunction unless a doctor prescribes those drugs for FDA-approved secondary use, such as hypertension. |
| Birth Control (including IUDs) | AHCCCS will provide coverage for birth control and other forms of family planning, such as IUDs. |
| Fertility Treatment | Arizona Medicaid will not pay for fertility treatments. |
| Specialist Services | |
|---|---|
| Arizona Medicaid will generally cover specialist visits if you receive a referral from your primary care physician. Depending on the service and what kind of AHCCCS plan you have, you may need to make a co-payment when you see a specialist. | |
| Dermatology | Arizona Medicaid will cover medically necessary dermatological treatments for skin conditions. |
| Physiotherapy | AHCCCS will cover necessary physical therapy treatments after injury or surgery. |
| Massage Therapy | AHCCCS will not cover massage therapy unless it is part of a medically necessary and doctor-prescribed physical therapy regimen. |
| Podiatry and Foot Care | AHCCCS will provide podiatric care that is medically necessary. |
| Allergy Testing | Allergy testing and allergist appointments are covered by AHCCCS pending a referral from a primary care physician. |
| Sleep Physician Services and CPAP Machines | AHCCCS will cover medically necessary equipment, such as CPAP machines. |
It is also important to note that AHCCCS does not cover the cost of funerals. While the state offers basic resources and very limited monetary benefits towards burial costs, what is available will most definitely not cover the rising burial costs and services. It is always wise to ensure that in the event of your passing, your family is secured with comprehensive funeral insurance .
Arizona Medicaid exists to help low-income families and individuals receive the medical care they need. However, there are several things that Arizona Medicaid will not cover that could still be medically relevant. In those cases, a private health insurance plan can fill the gaps and provide coverage Arizona Medicaid does not.
For example, your Medicaid plan may not cover the long-term care you need after an illness or injury. In this case, a long-term care insurance plan can provide the funds so you can get the necessary treatment. Other types of private insurance, such as life insurance, can help pay for medical costs Medicaid will not cover, especially in the event of your passing.
There are no laws preventing Arizona citizens from having both Medicaid and private health insurance. If you have a work-sponsored healthcare plan, you can still qualify for Medicaid coverage if you are below the necessary income limits. If you do have Medicaid and private insurance, you will have to go through private insurance first before Medicaid will cover the remainder.
Insurdinary makes finding the right private insurance carrier for you easy with experienced insurance agents and the ability to compare insurance quotes in one place. If you’re ready to add private health insurance to your medical experience, contact Insurdinary today for a free, no obligation health insurance quote.
Insurdinary, and its network of partners offer many different types of insurance. In addition to health, dental, disability, life, funeral and travel insurance as discussed on this page, you may also be interested to explore the following: