MENUMENU
The Texas Medicaid insurance program provides healthcare coverage throughout the Lone Star State, including long-term services and support. Discover everything you need to know about the program, including what it covers, who is eligible, and how to apply.
Residents must meet various income, age, or disability requirements to qualify for coverage through Texas Medicaid, also known as Texas STAR. As of June 2023, 5,881,947 Texans were enrolled in Medicaid. However, the state has completed its “unwinding” process due to the pandemic and nearly 2 million of those people are no longer covered under the program.
Extending your healthcare coverage through a third-party insurance provider makes it possible to receive the same level of healthcare services, and you may be surprised at how affordable plans from private insurers are. This guide will help you understand the ins and outs of Texas's Medicaid program and when to consider purchasing extended coverage to fulfill all of your healthcare needs at an affordable cost.
Texas STAR stands for State of Texas Access Reform and is the name of the Texas Medicaid program, which provides affordable health insurance coverage for low-income individuals and families. The Texas STAR Medicaid service covers a wide range of mental and physical health services, including hospital stays, behavioral counseling, and prescription drugs.
The plan also includes coverage for dental and vision care. Eligible residents can easily treat any pre-existing conditions at little to no cost through Texas Medicaid.
Health benefits for Texas residents are typically free of charge, though you may have a co-pay for some services, depending on the type of care and form of coverage. For example, the Children's Health Insurance Program, an alternative to Texas Medicaid, requires upfront payments for various services. The amount of each co-pay depends on the federal income poverty limits, but the co-pay for most prescriptions and non-emergency doctor visits is around $35 or less.
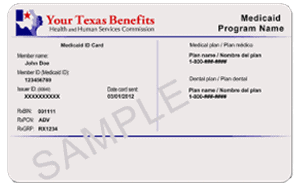
When you are approved for Medicaid benefits, you will get a Medicaid card. This includes information about your health plan and an ID number that providers use to confirm your benefits. Keep this card in a safe place at all times, and be sure to bring it to all healthcare appointments so your doctor can accurately log your insurance information.
If you're wondering how to apply for Texas STAR benefits, you have a few options. If you are an eligible resident, you can apply in person at a local Texas Health and Human Services office. You will need to bring proof of identity, citizenship, and income, so gather the necessary documents before heading to a nearby office.
If you prefer not to apply for benefits in person, you can also do so in the following ways:
Once the Health and Human Services Commission receives your application, it can take up to 45 days to process your request. You can call 211 for updates regarding your application during that time.
You must meet a certain set of criteria to qualify for Medicaid services in Texas. This includes being a resident of the state and either a U.S. national, citizen, permanent resident, or legal alien. You must fall under various income thresholds depending on the size of your household.
In addition, you need to fit into one of the following categories to be eligible:
Once the Health and Human Services Commission approves your application, you will be able to select a health plan from one of Texas STAR's managed care organizations. Sixteen contracted insurers partner with the Texas Medicaid program to supply benefits to residents, including Blue Cross and Blue Shield of Texas, Aetna Better Health, and Molina Health Healthcare of Texas. You can choose a health plan depending on your location and the providers you use.
If you're enrolled in Texas STAR benefits, you can change your health plan at any time. A change to your plan will require you to apply for a new ID card. You will receive your Medicaid card in the mail after your application is approved and the enrollment process is complete.
Do you need to renew your card or request a new one? You can visit Texas's online patient portal at YourTexasBenefits.com and click "Manage" once you log in to your account. From there, select "Medicaid & CHIP Services" from the Quick Links section and then "View Services and Available Health Information."
The screen will give you the option to select a different Medicaid client. Do this and then click "Cards" and "Order Card." You will need to confirm your mailing address to receive your updated card.
You may also call (800) 252-8263 to request a new card. You'll need to provide your Texas STAR plan number in order to fulfill your request.
What is Texas STAR coverage good for? If you have Texas Medicaid coverage, you can receive free treatment from different healthcare providers. Discover what types of services and treatment you can receive as a Texas STAR plan holder.
Dental benefits are available through the Texas STAR plan to cover twice-a-year cleanings and oral exams for pregnant people and adults over the age of 21. You can also receive X-rays once a year, non-surgical extractions, and the following emergency dental procedures:
Children who receive Medicaid benefits through Texas's Children's Health Insurance Program (CHIP) also have coverage for annual cleanings, exams, and X-rays, plus special dental services like fluoride and sealant treatment. Tooth extractions, fillings, and certain oral surgeries are also included in coverage, while orthodontic services like braces and retainers need prior authorization.
If you hold Texas STAR insurance, some prescription drugs are available at no cost. Texas is one of the states that use a uniform preferred drug list among all managed care organizations. In other words, you have access to the same type of prescription drugs no matter which of the state's 16 health plans you use.
Some of the medications that are available under Texas Medicaid's preferred drug list include:
The Health and Human Services Commission may add or remove medications from this list at any time. Be sure to check your coverage before picking up a prescription. If you do not have coverage, ask your doctor if it's possible to use an alternative drug to treat your condition.
You can receive treatment for behavioral and mental health conditions through Texas Medicaid. This includes inpatient and outpatient psychiatry services, substance abuse counseling and treatment, and mental health rehabilitative services. Confirm that your provider accepts Texas STAR insurance before seeking mental health treatment.
Investing in quality disability insurance is an excellent way to assist with some of the costs incurred with not being able to work either temporarily or permanently, and to help with the cost of medical needs.
Texas Medicaid requires you to live in the state to receive coverage. Therefore, if you move to a different state, your Texas STAR benefits will be invalid, and you'll have to apply for your new state's Medicaid program. However, there are some exceptions when your Texas STAR coverage will extend to treatment in different states.
Texas STAR will cover the cost of your care if you face a life-threatening situation while traveling and need emergency healthcare in a different state. Another way it's possible to get out-of-state coverage is if you live near the border of another state and seek treatment at a preferred facility that accepts Texas STAR coverage. Confirm your coverage through your health plan before pursuing any type of non-urgent out-of-state care.
If you travel outside of Texas or the country for leisure, it’s highly recommended to invest in proper travelers insurance.
Students and children under the age of 18 can receive low-cost health insurance through two distinct programs. Children's Medicaid provides benefits to children in low-income families who fall below the income threshold. The Children's Health Insurance Program provides most of the same coverage as Children's Medicaid and is an affordable option for families who need insurance but earn more than the Medicaid requirements.
Families who have coverage through CHIP and Children's Medicaid have access to many medical services, including hospital stays, doctor and dentist check-ups, lab tests, X-ray imaging, and mental health services. Children's Medicaid offers these services with no co-pay, while CHIP plan holders will have to pay a small co-pay for each service. Children's Medicaid also covers long-term services for children with disabilities, but CHIP does not include this type of care in its coverage.
Seniors over the age of 65 who receive Medicaid services are eligible for the state's STAR+Plus program. This is a Texas Medicaid-managed care program that provides long-term services and support for both seniors and adults over the age of 21 with disabilities. Long-term care coverage is available through three different categories:
If you are an eligible senior, the STAR+Plus program connects you with a care coordinator. This person will meet with you within 30 days of your enrollment and discuss your goals and needs. They will then work with your providers and caregivers to ensure you receive the care you need.
Children and seniors are eligible for no-cost healthcare services through Texas Medicaid, but other groups may also qualify for coverage. Discover what other subgroups can join the Texas STAR program.
Medicaid programs across the country, including Texas STAR, are available for recognized American Indians and Alaska Natives. If you are a member of one of these groups, you will not have to pay any enrollment fees and have no out-of-pocket costs. To enroll, aboriginals must meet the requirements for Texas Medicaid and show proof of their tribal membership.
Veterans and active military members may enroll in either TRICARE or the VA health care program to receive health insurance benefits. If you're a military member and don't have coverage, you may also qualify for Texas Medicaid, depending on your income. Any dependents who have no coverage via a military insurance plan may be eligible for either Children's Medicaid or CHIP benefits.
Now that you know what Texas STAR covers, let's go over some of the healthcare services that aren't eligible for benefits:
It is important to note that the state of Texas and its Medicaid program does not cover the cost of funerals. Some assistance may be available at the county level when no other options are available; however, that is specifically on a case by case basis and is not guaranteed. Given the rising cost of funerals and related costs, protect your family with comprehensive funeral insurance.
If you need to treat various medical conditions, it's important to know what Texas STAR covers. Here is a breakdown of common medical treatments and procedures and whether you can receive coverage through a state insurance plan.
| Dental | |
|---|---|
| X-rays and Exams | With any Texas STAR plan, you receive Medicaid dental benefits, including routine cleanings, exams, and X-ray images. These services are typically required one to two times a year to maintain good oral health. |
| Wisdom teeth | Texas Medicaid covers non-surgical tooth extractions. Wisdom teeth removal, however, is a surgical procedure and is not among the dental benefits members can receive. Some health plans offer discounts on additional dental services. For example, Texas STAR members who have a health plan through Community Health Choice can receive a 25% discount on dental services like wisdom teeth surgery. |
| Vision | |
|---|---|
| Eye Exams | Texas STAR does cover vision care, such as routine eye exams. These appointments allow you to undergo eyesight tests to determine issues with your visual acuity. Members under the age of 21 can get eye exams once every 12 months, while adults older than 21 may get an eye exam every 24 months. |
| Glasses | Young Medicaid members in Texas who are under the age of 21 can receive new glasses or contact lenses once every 12 months. These members can also receive replacement frames through their benefits. Adults over the age of 21 can also get one pair of new eyeglasses once every 24 months. |
| Laser Eye Surgery | This procedure primarily corrects nearsightedness, farsightedness, and blurred vision due to astigmatism. Texas Medicaid does not cover eye surgery that treats these conditions, so patients will either need to seek a different form of treatment or pay out-of-pocket costs for this procedure. |
| Surgery | |
|---|---|
| Rhinoplasty | Plastic surgery procedures like rhinoplasty are not included in Texas Medicaid coverage unless your doctor proves that it is medically necessary. In some cases, rhinoplasty is necessary for patients to breathe easier or to correct nose deformities. Members cannot receive benefits if they schedule this procedure for cosmetic purposes only. |
| Breast Reduction | Texas STAR plan holders also need authorization to receive coverage for breast reduction surgery. A provider must declare it medically necessary before you can proceed with the treatment. Times when this procedure may be medically necessary include if you suffer from associated back pain that you can't treat another way. |
| Hospital | |
|---|---|
| Hospital stays | If you require care at an in-network hospital, your Medicaid benefits will cover the costs. This includes everything from overnight stays to emergency room visits and diagnostic testing like labs and X-rays, but you may have a co-pay of up to $125. |
| Ambulance transportation | Texas STAR covers the costs of emergency ground and air transportation. |
| Giving birth | Pregnant women can receive no-cost maternity care at in-network hospitals. This includes hospital stays for giving birth as well as newborn care. |
Behavioral and mental health services are available free of charge under Texas Medicaid when you go to a provider that accepts your health plan. You may receive services like inpatient and outpatient psychiatric care to treat mental illnesses. Coverage includes substance abuse counseling and does not require a doctor's referral or prior authorization.
Children who are eligible for Texas STAR can obtain counseling to diagnose a mental disorder, and adults can receive the same benefits to treat a known mental health condition.
| Sexual Health | |
|---|---|
| Gynecologist | Women with Texas STAR coverage can receive reproductive healthcare services at a gynecologist without a referral. Coverage includes prenatal care for pregnant women plus female health treatments like Pap smears or mammograms. |
| Erectile Dysfunction | Medicaid health plan providers do not cover erectile dysfunction medication on their preferred drug list. |
| Birth Control | Medicaid's Family Planning Services include coverage of birth control medications, including daily pills and intrauterine devices. Emergency contraceptives like the morning-after pill do not fall under this coverage, however. |
| Fertility Treatment | Texas STAR does not cover any fertility treatments, such as in-vitro fertilization or artificial insemination. |
| Specialist Services | |
|---|---|
| Dermatology | A dermatologist can treat issues with your skin. This specialist visit is free for Texas STAR members, as well as any testing or surgery the dermatologist may perform, such as biopsies. |
| Physiotherapy | Physical therapy falls under Texas's Medicaid coverage as long as you have a referral from your primary care doctor. You will most likely need to work with a physiotherapist to regain strength after an injury or improve your motor function after suffering from medical conditions like a stroke. |
| Massage Therapy | Massage therapy falls under Medicaid coverage as long as it is part of a prescribed therapeutic plan to treat a medical condition. Massages without prior authorization are not eligible for benefits. |
| Podiatry and Foot Care | Texas Medicaid covers visits to a podiatrist for all types of treatment related to the feet or ankles. |
| Allergy Testing | Like other specialists, allergists will accept Medicaid, but you will need a referral from their doctor. |
| Sleep Physician Services and CPAP Machines | Texas STAR covers sleep studies and CPAP machines to treat sleep disorders. |
Whether or not you are eligible for Medicaid benefits in Texas, you should consider a third-party insurance provider to give you the coverage you need. Not all services and procedures are available for Medicaid plan holders in Texas, but extending this coverage through a third-party company ensures you receive necessary medical treatment at an affordable cost.
Insurdinary can help you search for extended health coverage as well as disability, life, and travel insurance, among others. The Texas STAR program provides excellent benefits for eligible residents, but all Texans deserve access to quality healthcare with no coverage gaps.
We help make that possible by comparing state plans and coverage from other insurance providers so you can make the best decision for you. Let Insurdinary find you the ideal health insurance plan that won't leave you with outrageous medical costs. Fill out our convenient online request form to receive quotes for suitable insurance plans.
Insurdinary, and its network of partners offer many different types of insurance. In addition to health, dental, disability, life, funeral and travel insurance as discussed on this page, you may also be interested to explore the following: